EDITOR’S NOTE: AI-assisted editing tools were used only for proofreading and language refinement; all analysis, interpretation, and conclusions reflect the author’s original work.
Artificial intelligence (AI) has swept into clinical documentation faster than most of us expected. It can summarize a visit, flag a diagnosis, even suggest how a note should read. But for all that promise, the system still relies on us to keep it honest.
Efficiency – shorter notes, predictive dashboards, auto-coding – only matters when people stay in charge. Without that steady human check, algorithms can twist nuance, miss intent, or quietly rewrite a patient’s story. The real issue is no longer what AI can do for healthcare; it’s how we keep human judgment in command of the record.
Federal agencies have begun saying the same thing aloud. In early 2024, the Office of the National Coordinator for Health Information Technology (ONC) issued a rule requiring developers to disclose exactly how their “predictive decision-support interventions” operate within certified electronic health record systems. The agency acknowledged that any tool capable of drafting or suggesting documentation is already influencing clinical care. Around the same time, the U.S. Department of Health and Human Services (HHS) Office of Inspector General (OIG) updated its General Compliance Program Guidance, warning that automation without human supervision can spread errors faster than people can correct them. Both agencies reached the same conclusion: once an algorithm touches the chart, responsibility for what appears there still rests with the human signer.
By the fall of 2025, the question had reached Washington, D.C. The American Hospital Association (AHA) wrote to the White House Office of Science and Technology Policy, urging leaders to keep clinicians “in the decision loop” for every algorithm that affects care or coverage. Speaking for nearly 5,000 hospitals, the AHA argued that insurer-driven AI has already “exacerbated inappropriate denials,” piling new administrative work onto care teams.
It asked that a qualified clinician review every denial generated by a machine before it counts. The takeaway was plain: speed is no substitute for judgment. Whether it’s documentation or payment, AI can lend a hand, but it cannot act alone.
At the bedside, this debate feels personal. Physicians and nurses now type into records that anticipate their next word. Auto-filled differentials, templated assessments, and predictive phrases appear before the patient leaves the room. What was sold as timesaving often creates a second job: editing what the computer thought they meant.
Every suggested diagnosis or “smart” summary still needs a moment of clinical reasoning. If a note misrepresents the encounter, liability doesn’t disappear into the algorithm; it lands on the provider who signed it. Regulators have already confirmed that AI-generated entries carry the same legal weight as human ones. A hallucinated diagnosis, once accepted, can ripple through billing, quality metrics, and audits. In effect, clinicians now supervise both patients and programs.
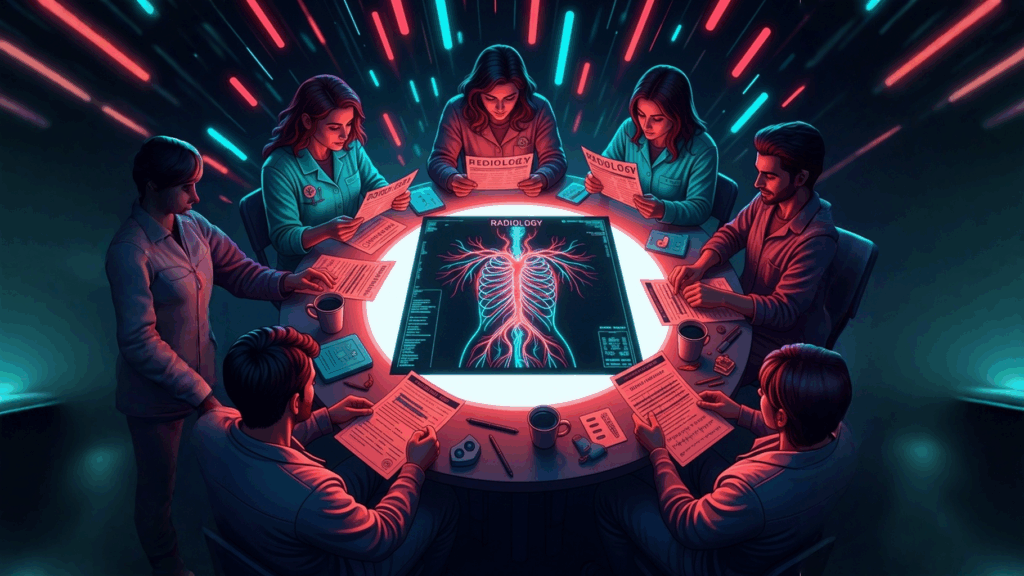
Clinical documentation integrity (CDI) and coding specialists feel a different version of the same pressure. Their tools highlight “possible sepsis,” auto-populate secondary conditions, or surface “documentation opportunities.”
Helpful? Often. Infallible? Never. The Office of Inspector General (OIG) cautioned that unexamined automation can “amplify inaccuracies in the health record.” The Office of the National Coordinator for Health Information Technology (ONC) coined a term for the slow creep of these edits – automation drift – when machine-written phrases pile up until the record no longer matches reality. After years spent fighting documentation creep, CDI teams are facing its digital cousin, moving at algorithmic speed.
Human checkpoints are the only real counterbalance. CDI and coding professionals verify that every AI-influenced statement still fits the patient’s story. A query that once clarified borderline diagnoses now also serves to test the machine’s suggestion.
When a CDI reviewer pushes back on a diagnosis that lacks indicators, they’re not nitpicking; they’re protecting compliance, accuracy, and the provider’s intent.
Revenue integrity depends on the same vigilance. One AI-prompted code can shift a case-mix index (CMI), an APR-DRG, or a Hierarchical Condition Category (HCC). If that entry isn’t supported, the claim becomes an easy target for denial.
The AHA 2025 warning captured this perfectly: payer algorithms are now auditing provider algorithms, and humans must reconcile the difference. It’s a loop no software can close on its own.
Breaking that loop requires three things: governance, transparency, and education. Governance means including AI oversight in every phase of the revenue cycle, not just IT. Transparency means labeling what the computer wrote and what the clinician wrote, so accountability stays visible. And education means teaching everyone involved – clinicians, CDI staff, coders – how these systems make their predictions and where they can go wrong. A patient’s chart should always read as the clinician’s voice, not the algorithm’s echo.
Keeping humans firmly in the loop finishes the job. Every AI-suggested diagnosis, query, or denial must be reviewed by a human before it becomes part of the legal or financial record. CDI specialists, coders, and clinicians share that duty; it’s where integrity meets compliance.
As automation deepens its reach, the line between help and authorship blurs. AI can find patterns, fill in blanks, and speed up routine work, but it can’t take on responsibility.
That remains with the people who review, interpret, and sign the note. For providers, it means documenting care, not code. For CDI and coding teams, it means defending accuracy against automation drift.
And for hospitals, it means weaving AI governance into every layer of compliance, quality, and education. Artificial intelligence may learn from us, but the standard of integrity must always remain human.