In 2019, I had an employee health exam, and fortuitously but startlingly discovered I had no sight in my left eye. I rushed my butt to an ophthalmologist, who determined that I had a macular hole (Diagnosis code H35.342).
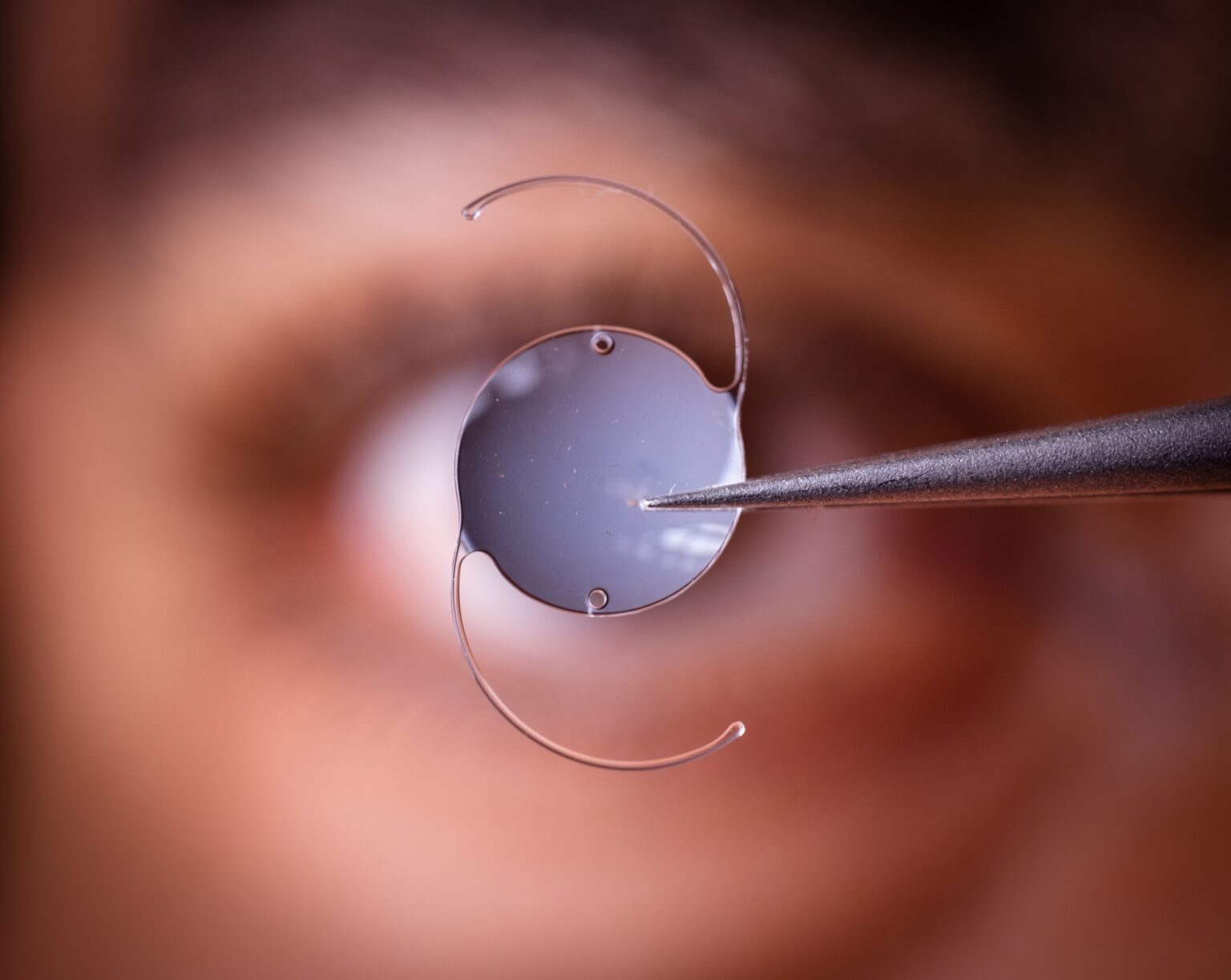
The repair experience (American Medical Association/AMA CPT®: 67042-LT) is one I never wish to go through again, but some sight was fortunately restored. As predicted, one year later, I had a cataract. So, in 2020, I had the interocular lens implant (AMA’s CPT: 66982-LT). What wasn’t predicted at that point was what was in store for me five years later: an “after-cataract.”
The primary ICD-10-CM codes for posterior capsule opacity (or after-cataract) are in the H26.4- category, with specific codes for the affected eye, such as H26.41 (right eye), H26.42 (left eye), and H26.43 (bilateral). These codes reflect posterior capsule opacification, which is considered a form of a secondary cataract.
Posterior capsule opacity (PCO), “after-cataract” or “secondary cataract,” is a common complication that occurs after cataract surgery, causing blurred or cloudy vision because the membrane holding the artificial lens becomes cloudy. My ophthalmologist described it “as wrinkly food wrap on the back of your lens.”
This happens when the lens epithelial cells that remain after surgery grow and multiply, forming a cloudy layer on the posterior (back) part of the capsule. It is not a new cataract, but a clouding of the capsule behind the new lens.
Symptoms include the following:
- Cloudy or blurred vision;
- A decrease in vision quality;
- Streaks or glare around lights;
- Haloes around lights;
- Increased sensitivity to light; and
- Trouble reading.
I had all of them!
The problem is treated with a quick, painless Yttrium Aluminum Garnet (YAG) laser capsulotomy procedure that creates an opening in the cloudy capsule (that wrinkly wrapping paper), restoring clear vision.
- The procedure is fast, painless, and effective, allowing light to pass through unobstructed and clearing the vision. By fast, I mean, four minutes!
- The recovery time for a YAG laser capsulotomy is typically very short, with some patients noticing an immediate improvement, while others may take up to 24 hours to experience the full benefit. It was noticeable to me within four hours. Vision was clear and bright.
- Most people can resume normal activities, including work, the day after the procedure. I was noncompliant and returned to work that same day! (Diagnosis code: Z91.198 Patient’s noncompliance with other medical treatment and regimen for other reason).
The AMA Current Procedural Terminology® (CPT) code for YAG laser capsulotomy is 66821-LT.
Description:
- Discission of secondary membranous cataract (opacified posterior lens capsule and/or anterior hyaloid); laser surgery (e.g., YAG laser)
This is a one-time procedure. Side effects from the YAG procedure include some mild eye irritation and floaters. I had both, and a dry eye. I just added some Thera Tears® and the dryness was gone. The floaters can last up to eight days. They were still present and annoying me at six days.
So, what are the procedure costs?
Per the American Society of Cataract and Refractive Surgery:
- Out-of-pocket cost ranges from 1,300-$4,000;
- Ambisurg facility Medicare payment is approximately $295; and
- Medicare physician payment ranges from $270-$453, depending on Medicare Administrative Contractor (MAC), geographic practice cost index of the physician’s location, and other factors.
I haven’t received the Explanation of Benefits (EOB) yet, so I can’t tell you whether these numbers need to be adjusted.
PCO is common. The incidence rates vary by study, but generally show 11.8 to over 28 percent of patients developing PCO within the first five years after cataract surgery. The incidence can be as high as 50 percent for adults and 100 percent for children over several years post-surgery.
Some key statistics include the following:
- Within one year: Rates can range from less than 5 percent to approximately 18.4 percent;.
- Within three years: The incidence can be around 20.7 percent; and
- Within five years: Over 25 percent of patients may develop PCO.
Factors affecting incidence include:
- Age: PCO occurs more frequently in younger patients due to a higher number of lens epithelial cells (LECs) and greater mitotic activity; and
- Surgical Technique:Improvements in surgical techniques and intraocular lens (IOL) design have influenced the rates of PCO. Although posterior capsule opacification (PCO) is one of the most common problems following cataract surgery, anterior capsule opacification (ACO) also occurs, but somewhat less commonly.
Both conditions represent the anatomic correlate of a secondary cataract (SC). As capsule opacification increases, the patient notices a decrease in vision that can lead to functional impairment. The approach to the management of functional impairment due to SC, whether the result of ACO or PCO, or both, is like that of functional impairment due to cataract.
Treatment of SC is reserved for those patients who have documented functional impairment that impacts their ability to perform needed and desired activities of daily living.
Beyond YAG, there are other surgical options to treat PCO and other visual impairments. These are just a few and include the following:
a. Microsurgical Capsulotomy: (AMA’s CPT: 66999);
b. Implantable Collamer Lens (ICL): (AMA’s CPT: 66985);
c. Anterior Chamber Lens (ACL): (AMA’s CPT: 66985);
d. Chemical Treatment: (AMA’s CPT: 66030); and
e. Other Procedures:
- In rare cases, other procedures such as vitrectomy or lens exchange may be considered as alternatives to YAG laser capsulotomy.
Posterior capsule opacity is a common and treatable complication of cataract surgery. With the simple YAG laser procedure, most patients quickly regain clear vision and return to daily life.
It’s important to note that the best alternative for a specific patient will depend on factors such as the severity of the PCO or their eye condition, the patient’s overall health, and their preferences.
Consult with an ophthalmologist to discuss the available options and determine the most appropriate treatment plan.
EDITOR’S NOTE:
The opinions expressed in this article are solely those of the author and do not necessarily represent the views or opinions of MedLearn Media. We provide a platform for diverse perspectives, but the content and opinions expressed herein are the author’s own. MedLearn Media does not endorse or guarantee the accuracy of the information presented. Readers are encouraged to critically evaluate the content and conduct their own research. Any actions taken based on this article are at the reader’s own discretion.